What is Azoospermia?
It is the situation where no sperm cells can be seen in the semen sample given. It is seen in 1% of the society, but in 10-15% of couples who apply to us because they cannot have children. In some of the azoospermic patients, there is no or less sperm production (b), and in some of them, sperm production is sufficient, but there is no sperm in the semen due to obstruction in the sperm ducts (obstructive azopermia).
Treatment in Male Infertility
Treatment planning is made according to the problem determined after the examinations. Microscopic varicocelectomy is recommended in the presence of varicocele, and medical treatment is recommended in hormonal deficiencies.
Hormone Therapy in Male Infertility
The 2 hormones related to sperm production in the testicles are FSH and LH, which are produced from the pituitary gland in the brain. FSH stimulates Sertoli cells in the testis and stimulates sperm production. LH, on the other hand, activates the production of testosterone by stimulating the Leydig cells.
These hormones can be given externally in the treatment of azoospermia due to insufficient sperm production in the testis or in the absence of hormone production from the pituitary (hypogonadotroic hypogonadism). Klinefelter Syndrome also constitutes the patient group who benefit from hormone treatments. These treatments are applied by monitoring in 3-6-12 month follow-ups.
Vitamins, anti-oxidants and food supplements are also used to support hormone therapy.
What are the Conditions that Negatively Affect Sperm Quality? What should couples who want children pay attention to?
Although sperm production in men continues at every age, there will be a decrease in sperm count and quality with advancing age. Apart from this, the sperm production process is affected by many negative environmental factors. The most known ones are exposure to cigarette smoke (direct smoking or being in a smoking environment), obesity, stress, exposure to chemical substances (especially for those working in the paint industry), working in extremely hot environments (mining, iron-steel, bath-sauna workers), direct or Inflammatory diseases that indirectly affect it (orchitis-ovarian inflammation, mumps, covid-19, urethritis-gonorrhea, tuberculosis-tuberculosis), egg failure, varicocele, testicular tumor-surgery, chemotherapy, radiotherapy can be counted.
Couples who want to have children should especially pay attention to their diet, stay away from stress, rest well, do sports and stay away from cigarette smoke.
What are Assisted Reproductive Methods?
Assisted reproductive methods are recommended for couples who cannot conceive naturally. These treatments can be counted as sperm infusion into the uterus (intra uterine insemination; IUI), ovulation-regulating treatments (ovulation induction) or in vitro fertilization (IVF; ICSI) and advanced fertilization treatments.
- Vaccination is the transfer of the sperm of the man into the uterus of the woman after being given hormones and cracking. Thus, more sperm and eggs meet unhindered and the chance of fertilization is increased. With this method, there is a monthly success rate of around 15% and it can be tried for 3-4 months. In couples with low sperm count, 3-4 sessions can be tried, but if unsuccessful, IVF should be tried.
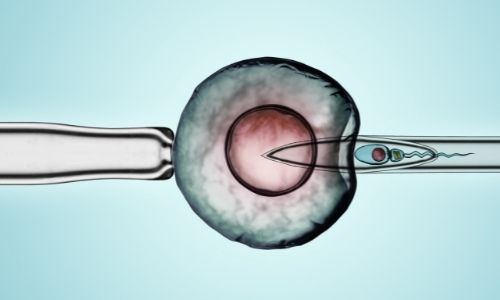
-The other treatment method is IVF (in vitro fertilization), which is popularly known as the in vitro fertilization method. With this method, ovulation is provided with drugs and mature eggs are taken out of the body with a process called OPU (oocyte collection). Under laboratory conditions, an embryo is created by injecting the sperm into the egg (ICSI). Developing healthy embryos are selected and injected into the mother's womb.