What is Prostate?
The prostate is one of the male reproductive organs. It is the largest gland of the organs.
It consists of secretory cells (tubuloalveolar glands) and their supporting tissue.
It weighs 18-20 grams.
The prostate is one of the male reproductive organs. It is the largest gland of the organs.
It consists of secretory cells (tubuloalveolar glands) and their supporting tissue.
It weighs 18-20 grams.
The prostate is an organ that exists in every man. It is an organ that surrounds the urethra just below the bladder. Its shape and size are similar to chestnuts.
On the outside, there is a shell tissue called capsule. Nerves that provide erection pass around it and spread towards the penis. Beneath it are the muscles (sphincter) that prevent us from incontinence.
It is shaped like an inverted pyramid. Its base fits over the opening of the urinary bladder. On its back is the rectum, the last part of the large intestine. The lower end part ends by tapering. The urethra, called the urethra, passes through it. It has a capsule (shell) consisting of collagen and elastin that surrounds it from the outside.
The secretory tissue makes up 70% of the prostate, and the supporting tissue called fibromuscular stoma makes up 30%. At the lower end, there is a channel called the verumontanum where the semen is expelled.
The prostate is anatomically divided into 5 layers. The transitional region surrounding the urethra (5%) and the region outside this region are the central region (25%).
Benign prostate enlargement usually occurs as a result of the growth of cells in the transitional region. The region surrounding these regions externally is the peripheral region (25%).
Prostate cancer usually originates in the peripheral region. Except for these regions, the anterior upper part of the prostate constitutes 30% and is called fibromuscular stroma. This region contains more muscle tissue.
90% of the fluid called semen that comes out after sexual intercourse or masturbation is produced from the prostate gland. Prostate secretions help sperm live in the female reproductive organs. Due to its location next to its secretory function, it also has a duty to control urine. The prostate is not a vital organ. There is a risk of deterioration of sexual functions and urinary control when taken.
The prostate is formed in male babies by the stimulation of male hormones in the womb. It does not change in size after birth until puberty. At puberty, it begins to increase in size with hormonal stimulation. It is around 20gr in an adult male.
After the age of 40, the growth of the prostate gland accelerates as a result of hormonal imbalance. It can cause complaints by compressing the urinary tube passing through the middle.
The job of the prostate is to produce semen. About 10% of the semen is produced in the testicles, 60% in the seminal vesicle, another gland behind the prostate, and 30% in the prostate.
Prostate secretion makes semen alkaline. Thus, sperms are protected from the acidic environment in the vagina. Prostate secretions cause the semen to become thick and sticky and then to become fluid.
During sexual intercourse, the semen is stuck in the female genitals in a dark sticky state. Then, by becoming fluid, the sperms are activated and fertilization is ensured.
The prostate gland is an organ that is sensitive to the male hormone testosterone. It is present in men of all ages. After the age of 40, it begins to grow as a result of hormonal fluctuations or some metabolic events.
Prostate cancer is the most common type of cancer in men after lung cancer. If cancer is suspected with a blood test called PSA and examination, prostate MRI (multiparametric prostate MRI) and biopsy are recommended for cancer diagnosis.
In recent years, our chance of success in diagnosing cancer has increased with fusion or smart biopsy, which is a special biopsy technique that we also apply. This subject is explained in detail in the prostate cancer topic.

The enlarged prostate tissue compresses the urethra.
Sometimes it even extends towards the urinary bladder (median lobe-middle lobe) and closes the urinary canal almost completely like a lid.
Difficulty urinating, impaired urine flow, weak urine, intermittent urination, frequent urination, getting up to urinate at night, feeling of incomplete emptying after going to the toilet, burning and bleeding in the urine can be seen.
Their complaints especially increase in cold weather and they may become unable to urinate over time.
Urine output is provided by inserting a catheter in patients with occlusion.
As in every patient, the patient's complaints and additional diseases are evaluated in detail. Prostate enlargement is not the only reason for lower urinary tract voiding complaints. It should not be forgotten that diseases that impair bladder contraction, diabetes, some neurological diseases, urinary tract stenosis, infections also cause similar complaints.
Therefore, patients should be evaluated in detail before treatment.
![]()
Urinalysis, detailed evaluation of bladder, prostate and kidneys with ultrasonography, urine flow measurement with urination test, PSA blood test are the basic tests. The urine remaining in the bladder after urination with ultrasound must be measured.
![]()
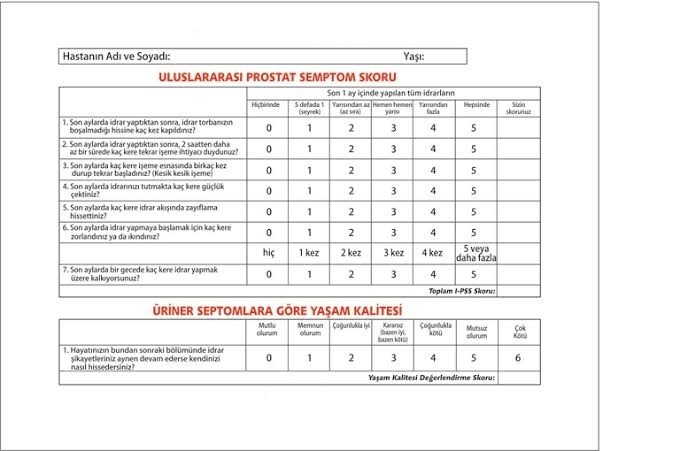
In addition, the International Prostate Symptom Score (IPSS), in which patients evaluate themselves, also helps us to evaluate the severity of complaints.
In some cases, it may be necessary to examine the urethra and bladder endoscopically (instrument with a camera).
This procedure can be performed in operating room conditions, or it can be performed in office conditions with a flexible cystoscope (a thin-camera device that can be bent).
Drugs that relax the urinary tract (alpha blockers) are given to reduce the complaints related to the enlarged prostate. The most common side effect of these drugs is the absence of semen output. When these drugs, which act by relaxing the muscles in the neck of the urinary bladder, are used, semen flows back into the bladder during intercourse and this is called retrograde ejaculation. This does not cause infertility. If you do not want to have children, there is no harm.
The second type of drug given to patients with a larger prostate (greater than 40ml) (5-alpha reductase inhibitors) prevents the conversion of testosterone to its more active form in the prostate. These drugs can cause erectile dysfunction.
Sometimes, patients with accompanying erectile dysfunction may be offered drugs (phosphodiesterase inhibitors) that will both relieve urinary complaints and improve their performance.
Another problem we encounter in our elderly patients with enlarged prostate is the deterioration in the smooth muscle structure of the bladder due to age or obstruction. In patients with involuntary bladder contraction (overactive bladder) and decreased bladder capacity, drugs that relax bladder smooth muscles (anti-muscarinics) may also be given.
The drug treatments described above may be used alone or in combination. This situation is decided by making a detailed evaluation.
Patients with an enlarged prostate become unable to urinate after concomitant infection, edema, anesthesia, stones in the bladder, chills or excessive fluid intake. Applications to the emergency department with severe abdominal-groin pain. On ultrasound, it is clearly seen that the bladder is full (globe vesical). First, the catheter is inserted by the emergency physician or urologist. Sometimes the prostate of the patients is very large and the probe cannot exceed the prostate and reach the bladder. In these cases, a probe extending from the skin to the bladder, called a percutaneous cystostomy, is applied under local anesthesia. Patients experiencing acute urinary retention are usually able to urinate after drug therapy. However, surgical treatment is definitely recommended in cases that are unable to urinate or recurrent retention after catheter removal.
The above-mentioned conditions are definitely patients who need surgery. Each patient should be evaluated individually. The most appropriate treatment method is chosen for the patient by considering many factors such as co-morbidities, medications, general health status, expectations from the surgery, sexual life, social-work life. The technical possibilities and surgical experience of the surgeon are also very important. The surgical techniques are briefly summarized below.