Testicular Cancer Treatment
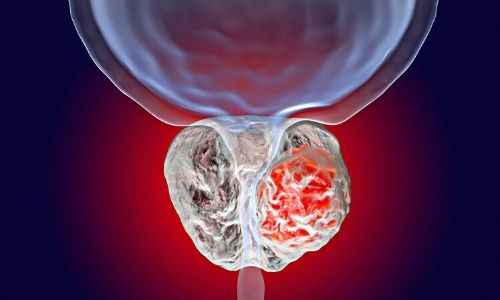
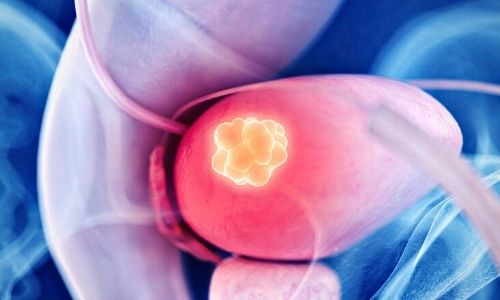
After the diagnosis of testicular cancer is made and the necessary examinations are made, the first basic treatment is the removal of the tumorous testis from the body, that is, orchiectomy. Under spinal or general anesthesia, with an incision made from the inguinal region, the testis and the cord extending from the groin to the testis are surgically removed as a block.
The process takes about 30-60 minutes. Testicular prosthesis can be placed during the procedure for patients who wish. This prosthesis is not functional. It only provides the appearance of the testis, that is, we recommend it to our patients in terms of cosmetics.
Again, preoperative sperm freezing (sperm-cryopreservation) is recommended for patients who want to have children in the future.
Postoperatively, patients are usually discharged either the same day or the next day. Patients can return to work after 1 week-10 days. It is recommended to avoid heavy lifting and heavy exercises for a few weeks. Sexual activity can be started after a few weeks.
Types of Testicular Cancer
The testicular mass removed by surgery is examined by pathologists. During this examination, detailed information such as the tumor's diameter, location, type, spread in the testis layers, and vascular-nerve involvement are obtained.
The most common type of testicular cancer is seminoma. It especially affects men between the ages of 30-45 and has a slow course, does not metastasize too much. Tumors other than seminomas are classified as non-seminomatous germ cell tumors and generally affect men aged 20-35 years more. Mixed germ cell tumors with tumor types other than seminoma and seminoma are also encountered.
Tumor types originating from cells other than germ cells are much rarer types.
The disease is staged by considering the pathology and radiology report and tumor markers. As a result of this staging, evaluation is made together in oncology councils where Urology, Radiology, Oncology and Radiation Oncology specialists participate together.
Early-stage seminomatous and non-seminomatous tumors confined to the testis are followed closely after surgery. Chemotherapy can be used as an alternative in patients who do not comply with the follow-up protocols.
Radiotherapy can be applied to patients with seminoma that has spread to lymph nodes in the retroperitoneal region. In some patients, chemotherapy and radiotherapy can be applied together.
What is the RPLND Process?
It is a surgical procedure in which persistent lymph nodes in the posterior abdominal wall are cleaned despite the chemotherapy given. It is an operation that requires meticulous surgery and experience. Today, we also apply it with laparoscopic or robotic surgery.
Does Testicular Cancer Negatively Affect Erectile Dysfunction?
Men diagnosed with testicular cancer are negatively affected psychologically. Sexual functions may be adversely affected by the psychology of losing an organ, fear of being infertile or masculinity. However, the applied surgery or the treatments given do not have a negative effect on penile erection mechanisms.
A single testicle can produce enough male hormones and sperm. Chemotherapy will negatively affect the sperm production of the remaining healthy testis. Therefore, preoperative sperm freezing is recommended for patients.
It should be noted that the effects of chemotherapy are temporary, even if the sperm is frozen.
Click for information and appointment.